February 9, 2021
Continuous glucose monitoring (CGM) devices have been in use for about 20 years, mainly by diabetics who rely on them to monitor life-threatening swings in their blood glucose levels. Within the past couple of years, however, these devices have slowly been making their way into the mainstream.
As I mentioned in last Saturday's podcast “A Rocket Scientist Homeschooler’s Insider Blood Glucose Monitoring Secrets, The Best Way To Use A Continuous Glucose Monitor (CGM), Blood Sugar Biohacking Tips & Much More!,” I myself have been using a CGM from time to time throughout the last four years—and have gleaned some very valuable information from it.
See, CGMs are extremely useful tools for accessing real-time feedback about how your body responds metabolically to what you eat. By measuring and displaying your circulating blood sugar, you can see how efficiently your body is able to deal with the carbohydrates in your meal as well as your lifestyle choices surrounding that meal. A spike on the CGM simply means too much circulating glucose, which can cause short-term mood and quality of life issues; long term, it can contribute to a wide range of conditions from acne to Alzheimer’s disease.
But, because metabolic health is ultimately about how all the cells in your body generate energy, CGM readings can tell you much more than just what your postprandial glucose response is. In fact, metabolic health interacts with just about every aspect of your life.
In today's article, you'll discover five areas beyond postprandial response where a CGM can give you insight: sleep, stress, exercise, alcohol, and weight loss. For each one, you'll learn how glucose interacts with your body and what might cause different readings on your CGM. By understanding all the factors that go into your CGM reading, you can use it to make better diet and lifestyle choices.
What Exactly Is A CGM?
A CGM is a small device that attaches to your body (typically your upper arm or abdomen region) for up to 14 days that takes ongoing measurements of circulating blood glucose. CGMs don't actually read your blood, rather the glucose in subcutaneous fluid just underneath your skin by using a tiny, imperceptible probe. The CGM has a transmitter that sends that raw data to your smartphone. There, software interprets it and gives you context for what you see by tying movement on a graph to your meals and lifestyle choices.
CGMs are useful because everyone’s metabolic machinery works differently: What causes a blood glucose spike in one person may elicit a less dramatic response in someone else. By tracking your individual reaction to food and lifestyle factors, you can work towards attaining normal glucose levels by making choices that work for you.
So, what are “normal” glucose levels?
When you get your blood glucose checked at your doctor’s office, it is typically via a fasting plasma glucose (FPG) test, which measures glucose levels in your blood after not eating for eight hours. The American Diabetes Association places fasting plasma glucose levels into three categories: “normal” (less than 100 mg/dL), “pre-diabetes” (100-125 mg/dL), and “diabetes” (more than 126 mg/dL).
However, these only measure your glucose at a single point in time. There are no standardized, universally accepted criteria for what “normal” 24-hour glucose values are using CGM technology.
As I mentioned earlier, CGM devices measure interstitial glucose levels (glucose from the fluid in between cells), compared to glucose in the blood measured in the FPG tests. While interstitial glucose and blood/plasma glucose levels correlate highly, they are not precisely the same, and diagnoses are not made from interstitial measurements. However, there have been a number of studies done on nondiabetic people wearing CGM devices, in which you can at least see trends. You should always consult a doctor for your specific targets, but below is a summary of a review of the research. This summary was compiled by the team at Levels Health (the company that makes the software I use to monitor my glucose levels, which you'll learn more about below).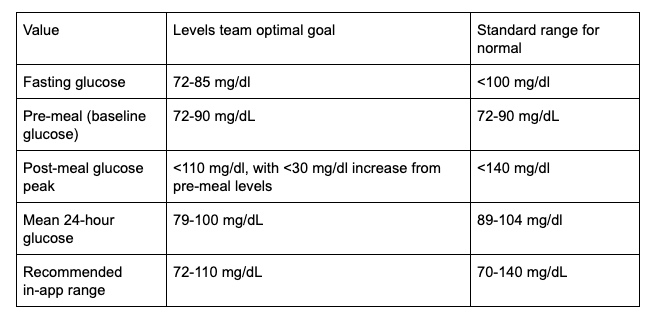
As you can see, the ranges are fairly similar, with Levels' optimal ranges for interstitial glucose being on the lower end, or, in the case of fasting glucose, having a bit more precise of a target.
Now, let's dive into the five areas beyond postprandial response that will show up on your CGM.
Sleep Quality
Sleep is intimately connected to metabolic health. While a few nights of sleep deprivation can throw off your body’s ability to process glucose efficiently, it’s not just a lack of sleep that can cause blood glucose problems.
Sleep quality also seems to have a significant impact on metabolic health. One study followed adult men for eight years and found that those who reported interrupted sleep and difficulty maintaining sleep had two to three times the risk of developing type II diabetes.
The regulation of glucose and insulin are partially controlled by cortisol, which tells your body that something “stressful” is happening and prepares you to have sufficient energy to utilize against whatever this real or perceived threat may be by mobilizing stored glucose from your liver into your bloodstream. Cortisol also decreases insulin production in your pancreas and reduces insulin sensitivity in your body, which means that the glucose is less likely to be utilized by cells and more likely to remain in circulation, thereby elevating blood glucose levels.
Cortisol levels tend to be lower during the evening and early part of the night, which means glucose levels tend to stabilize around a lower range at night. But, if you wake in the morning and see a series of peaks on your CGM, or elevated levels through the night instead of a smooth, low line, it’s possible that your sleep quality was off, leading to inefficient glucose processing.
What you can do?
Everyone’s metabolic responses to sleep are unique, but following basic sleep hygiene rules can help.
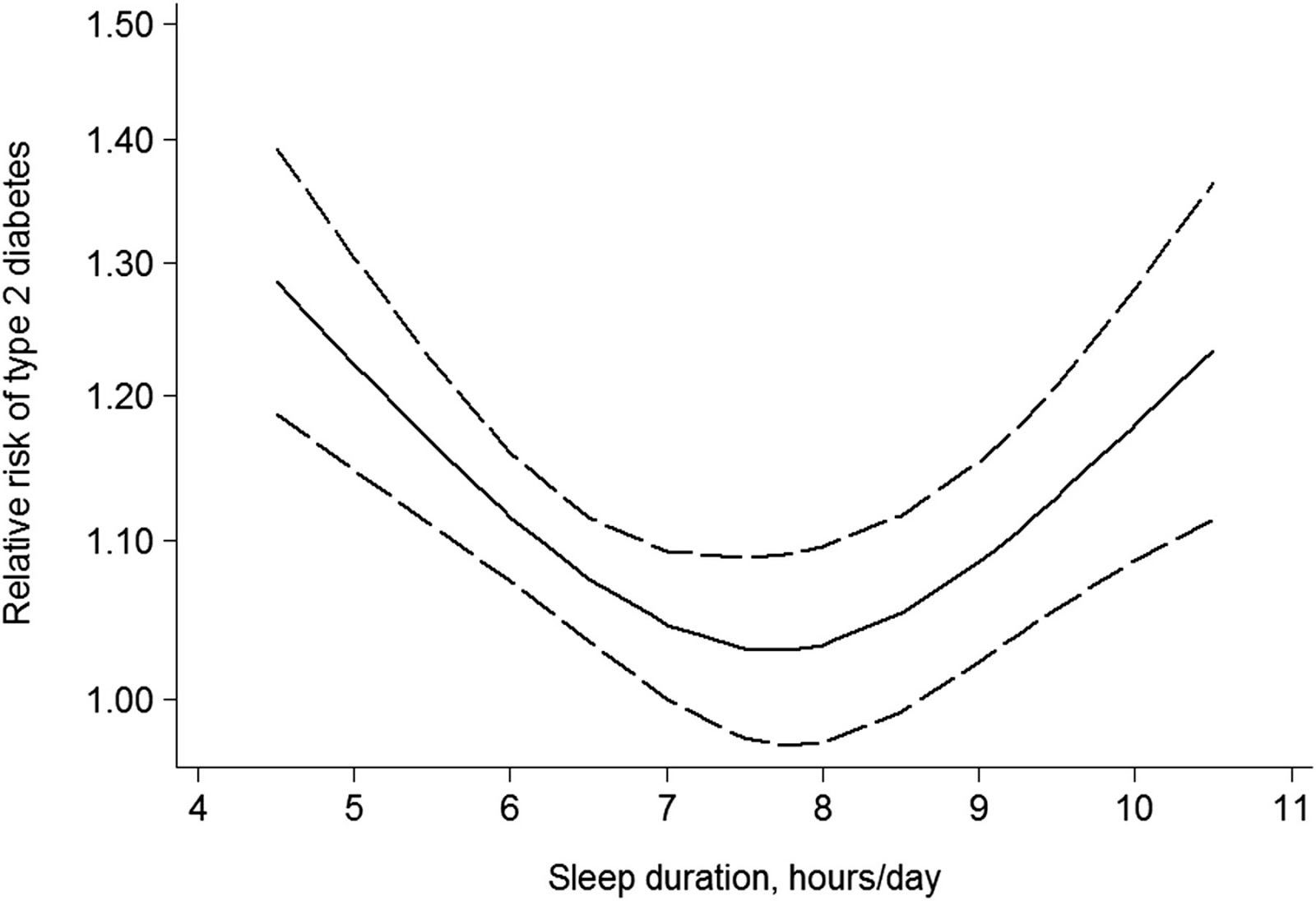 Get around seven to eight hours of sleep every night. As you can see in the graph to the right, any less than seven hours, your risk of diabetes increases sharply for every hour lost—above eight hours, the risk also increases.
Get around seven to eight hours of sleep every night. As you can see in the graph to the right, any less than seven hours, your risk of diabetes increases sharply for every hour lost—above eight hours, the risk also increases.- Try to get deep sleep. Research also shows that glucose levels decrease by an average of 5% during REM sleep, as compared to non-REM sleep stages, which may contribute to periodic dips seen at night in nondiabetic people. In fact, healthy people who have glucose dips below 70 mg/dl have twice as many dips at night as compared to during the day.
- Eat earlier in the evening. When you wake up after a long night’s sleep, your body has been in a fasting state for quite a few hours. During this fasting period, your body expends circulating and stored glucose to perform all the usual physiologic processes. If you tend to stop eating earlier in the evening and do not snack at night, this fasting window will be greater, and it may lead to lower glucose levels during that night.
- Skip the late-night drinks. As I'll discuss below, alcohol tends to lower glucose levels, especially if you’re fasting. If you’re seeing very low levels at night, have that evening glass of wine a little earlier.
For more resources on sleep, my articles “The Last Resource On Sleep You’ll Ever Need: Ben Greenfield’s Ultimate Guide To Napping, Jet Lag, Sleep Cycles, Insomnia, Sleep Food, Sleep Supplements, Exercise Before Bed & Much, Much More!,” “10-3-2-1-0: Five Numbers To Remember For Lulling Yourself Into A Deep, Restorative Slumber (Without Fancy Biohacks Or Supplements).,” and “Sabbath Ramblings: Now I Lay Me Down To Sleep (5 Key Principles For A Good Night’s Rest).” outline pretty much everything you need to know to get a good night of deep, restful sleep. For more information on cortisol, including foods and supplements that reduce it, read my article “Why We’re All Chronically Stressed (And How You Can Combat Stress With Food And Supplementation).”
Stress Response
Stress and metabolic health have a two-way relationship: Stress can affect glucose levels, but raised glucose levels can also affect your body’s ability to deal with stress.
Additionally, stress can cause you to overeat, which also raises glucose. Glucose spikes can lead to crashes as your body overcorrects to clear that excess glucose. Those crashes can cause fatigue, which leads to more stress. It's a vicious cycle, to say the least.
Studies show that perceived work stress alone can increase your circulating glucose levels, and in animal models, mice put under acute psychological stress took longer to clear a glucose load from their blood. Long term, the effects can be even more damaging. Elevated glucose requires your body to produce more insulin, which elevates cortisol and epinephrine, two hormones associated with the stress response. If those insulin levels are high for long enough, your cells can start to become “numb” to insulin’s effects. This is called insulin resistance, and it can lead to impairment of the negative feedback on the stress hormone pathways of the brain as well as an abnormal stress response in the brain, contributing to more stress, as well as depression.
What all of this means for anyone wearing a CGM is that, like sleep, stress can directly and indirectly cause you to see elevated glucose readings. If you see a spike, or elevated levels in general, that you can’t attribute to food, ask yourself if you’re feeling stressed. While it’s often difficult to tease apart individual effects, less stress in general will promote better metabolic health.
What can you do?
If you’re seeing a spike on your CGM you think is attributable to an acute stressor, the best thing you can do is calm yourself down with whatever works best for you, but some proven methods include breathing, meditation, exercise.
- Breathing – One study of insulin-resistant (type II diabetic) patients showed that people who did daily 20-minute diaphragmatic breathing exercises showed reduced fasting blood glucose and postprandial glucose levels within nine weeks.
- Meditation – In another study in individuals with heart disease, six months of twice-weekly meditation showed a significant decrease in fasting blood sugar, post-meal blood sugar, and hemoglobin a1c.
- Exercise – In Spark: The Revolutionary New Science of Exercise and the Brain, author John Ratey describes in great detail how exercise can significantly reduce stress, how it can be as effective as antidepressants, and how it's been shown in multiple studies to reduce stress and anxiety.
I have plenty of resources on breathwork, meditation, and exercise to explore on my site, but “How To Blast You (And Your Child’s!) Physical, Mental, & Spiritual Resilience Through The Roof With Breathwork.” outlines the exact breathwork and meditation routine me and my twin 12-year-old boys went through during quarantine. For more on the type of exercise you should be doing to support blood glucose control, keep reading.
Workout Intensity
Regular exercise is crucial to metabolic fitness. It can help train your body to be more metabolically flexible, allowing you to switch efficiently from using glucose for energy to burning fat. In addition, muscle contraction enables your muscles to take up glucose from your bloodstream without additional insulin. Finally, regular exercise can also increase the amount of fat you burn between meals as well as your number of cellular mitochondria (which process fat and glucose to make energy).
When you’re wearing a CGM, you’ll likely see different glucose responses from your body depending on the workout’s intensity.
Exercise that pushes your body above around 80% VO2max can lead to a spike similar to what you might see from eating something sweet. During intense workouts, glucose is your body’s primary energy source. So, once you’ve burned through circulating glucose, a hard effort stimulates your liver to release more of its stored glucose (glycogen) for energy. However, if what’s released exceeds what your muscles need, it can lead to higher circulating glucose, which shows up on your CGM.
You shouldn’t stress this kind of spike as you would a food-induced spike; it’s the result of a chain of physiological processes far different from your body releasing insulin to metabolize a meal. In one study, high-intensity training was shown to improve both fasting glucose and insulin sensitivity in as little as two weeks. Easy-to-moderate efforts such as walking, jogging, or taking a leisurely bike ride don’t require that quick glucose release from your liver. Your body can typically handle its energy needs with circulating glucose and by burning fat. So, if your CGM shows your glucose declining slightly or staying stable, you’re probably staying below around 60% of your VO2max.
What can you do?
The best advice for maintaining healthy glucose levels and insulin sensitivity is to exercise regularly, even if it is at low intensity. A recent study that compared high-intensity exercise three times a week with moderate exercise five times a week found that both produced better glucose control, but only on the days the subjects worked out. So, there is a greater benefit to working out more often, even if not as hard. In this particular study, moderate exercise was defined as 30-40 mins at 60% peak power output on a stationary bike. This same amount of moderate exercise (150 minutes per week) yielded greater longevity benefits and 31% less risk of dying compared with those who never exercised in another study.
Alcohol
What you’ll see on your CGM when you drink depends on several factors, namely whether you’ve eaten recently, are fasting, or are in a ketogenic state. Whether the alcohol is mixed with something carb-heavy such as juice or soda will also influence your readings.
For an average person having one or two non-mixed drinks, you likely won’t see much of a glucose effect. This is because of a sort of balancing act by your liver. It is thought that drinking alcohol decreases your liver’s ability to make new glucose (a process called gluconeogenesis), and while that can lead to lower circulating glucose levels, alcohol also stimulates the breakdown and release of stored glucose (a process called glycogenolysis) leading to a general stasis.
However, two factors can cause a more significant effect on your CGM. If you are fasting or in a ketogenic state, you may have lower stored glucose in your liver and muscles; and since alcohol inhibits gluconeogenesis, glucose levels can fall to dangerously hypoglycemic levels. In extreme cases, this can lead to seizures, coma, or death.
The other unique case is binge drinking, defined as five alcoholic drinks for men, or four for women, within two hours, even just once a month. In a study in rats, binge drinking for three consecutive days led to a state of rapid insulin resistance, which could last for more than two days after the drinking stopped. The drinking seemed to impair the brain’s ability to send signals to the liver about when to break down, make, or store glucose. Inflammation in the brain appeared to block the brain from receiving proper signals from circulating insulin. This effect on insulin would affect your body’s ability to clear the circulating glucose from your blood, leading to higher CGM readings.
What can you do?
- Sugary mixed drinks will lead to glucose spikes for nearly everyone, so it's best to avoid them altogether. Some people find sweet wines or carb-heavy beers like IPAs also lead to elevations. Experimenting with a CGM is the best way to find how your body reacts to your beverage of choice.
- Drink with a meal. One study suggested that drinking a small amount of alcohol (20 grams or about 1.5 drinks) before a carbohydrate-rich meal resulted in a 16% to 37% reduction in post-meal glucose. It is possible alcohol can trigger a rise in insulin sensitivity, though studies show variable findings.
- Keep consumption moderate. People who consume around one drink per day seem to have a lower risk of type II diabetes and higher insulin sensitivity. The reasons why aren’t fully clear yet, but a large meta-analysis of more than 10 studies showed moderate alcohol consumption resulted in decreased hemoglobin a1c levels and decreased fasting insulin levels.
I understand that occasional bouts of partying tend to be a societal norm, so if you've got a big event coming up where you know you may be partaking in heavy drinking—such as a wedding, vacation, or the end of a pandemic—read my article “Get Rid Of Holiday Hangovers Once & For All: How To Party Hard Without Doing Lasting Damage To Your Body.” to learn how to mitigate the effects of alcohol and never get a hangover again. If you're looking to cut down and need some “healthy alcoholic drink alternative” ideas, check out “Healthy Drinking 101: How To Make Feel-Good, Alcohol-Free Cocktails Chock Full Of Nootropics, Adaptogens & Botanicals!”
Weight Loss
Many people know by now that “calories in/calories out” is an overly simplistic model of weight loss that fails to account for the complex hormonal and biochemical pathways involved in energy balance, weight gain, and weight loss in the body.
The primary hormone involved in fat storage and weight gain is insulin, which tells your cells to take up glucose from your blood for energy; or, if there’s excess, storage.
Insulin is also your body’s primary anabolic hormone, which means it’s responsible for building things up rather than breaking them down. This anabolic (or storage) signal of insulin actually prevents your body from tapping into fat for energy. When you're not eating—in between meals, sleeping, or fasting—a lack of dietary glucose causes insulin levels to fall. This sends a signal to your body to burn stored energy, starting with glycogen. Once the stores of glycogen run out, you start burning fat. The goal of weight loss is to burn excess stored fat by mobilizing it and bringing it to parts of your body that can use it for fuel.
Therefore, you need to control your insulin to signal to your body that it should burn fat rather than store it.
A CGM can tell you a couple of things related to weight loss. First, because insulin tends to rise and fall with glucose, maintaining a stable glucose curve will prevent your body from producing excess insulin that can interfere with fat burning. Second, only when overall glucose is low can your body switch to burning fat. If your levels are elevated continuously, you can assume your body is not tapping into its fat stores.
What can you do?
- Don’t eat carbohydrates alone. Pairing carbs with healthy protein and fats can minimize glucose spikes. For example, If you eat an apple, pair it with a nut butter or put it in chia seed pudding.
- Skip processed foods of any kind. Foods made in a factory or that come in a package are likely to be refined (thus more likely to generate a glucose spike), be nutrient-poor, and have additives that can damage your metabolism and microbiome.
- Avoid refined sugar of any kind. Beware: There are dozens of hidden types of refined sugar in everyday foods ranging from ketchup to bread to salad dressings to peanut butter. If you have a sweet tooth, favor natural sweeteners such as stevia over artificial sweeteners like sucralose or aspartame.
For more on weight loss and blood glucose (and how they interplay with one another), read my article “The 2 Best Ways To Burn Fat Fast (Without Destroying Your Hormones Or Metabolism).”
“Fringe” Methods For Managing Your Blood Glucose Response
In addition to getting seven to eight hours of high-quality sleep, eating earlier in the evening, skipping those late-night cocktails, incorporating breathwork and mediation into your daily routine, getting in moderate exercise regularly, avoiding sugary mixed drinks, pairing carbs with proteins and fats, saying no to processed foods and refined sugars, etc., there are a few more “fringe” methods I'd be remiss not to include.
You can learn more about these in my recent podcast “A Rocket Scientist Homeschooler's Insider Blood Glucose Monitoring Secrets, The Best Way To Use A Continuous Glucose Monitor (CGM), Blood Sugar Biohacking Tips & Much More!,” but here is a quick rundown of five of my top “under the radar” strategies for managing blood glucose:
1. Heat – Intermittent hyperthermia has been shown to improve insulin sensitivity and reduce insulin resistance in obese mice. Insulin resistant diabetic mice were subjected to 30 minutes of heat treatment, three times a week for twelve weeks. The results were a 31% decrease in insulin levels and a significant reduction in blood glucose levels. This is one of the many reasons I start my day off with a sauna session. Basically, your blood glucose will go up during the sauna session, but long term will stabilize better after compared to if you weren't using heat.
2. Cold – As I covered in this article, cold thermogenesis increases your levels of brown fat, and a higher ratio of brown fat has been shown to increase sensitivity to insulin. Another study showed that people who spend hours in the cold daily exhibited an improvement in their control of blood glucose. Additionally, mice exposed to cold temperatures (39ºF) for two hours per day, five days per week for 14 weeks showed an improvement in glucose tolerance and enhanced insulin sensitivity. Unlike sauna, you'll usually see blood glucose plummet almost immediately and stay there for an impressive period of time in response to cold.
Check out my podcast “Fire & Ice: Tips, Tricks & Biohacks To Maximize The Benefits Of Sauna, Hyperthermia, Cryotherapy & Cold Thermogenesis.” for a comprehensive overview of how to start using both heat and cold.
3. Coffee – While a single cup of coffee or two can temporarily elevate blood glucose (a pretty transient rise and a healthy, normal stress response), higher habitual coffee consumption is associated with higher insulin sensitivity and a lower risk for type 2 diabetes. A Harvard University study tracked over 100,000 people for about 20 years and found that people who increased their coffee consumption by over one cup per day had an 11 percent lower risk of developing type 2 diabetes. Those who reduced their coffee intake by one cup per day increased their risk of developing diabetes by 17 percent. This appears to be an effect of coffee itself, and not caffeine, as caffeine has actually been shown to increase both glucose and insulin levels. So yes, decaf lovers, you too can enjoy these blood glucose benefits from coffee, even if you aren't getting the caffeine.
To learn more about coffee, including a deep dive into everything from sourcing to roasting the healthiest coffee you can find, read my article “23 Years Of Suckin’ Down Coffee: Tips, Tricks & Hacks I’ve Discovered For Getting The Most Out Of One Of The Safest Superfoods That Exists.“
4. Wild Bitter Melon Extract – This is one of the active ingredients found in Kion Lean. Along with Panax notoginseng and Astragalus membranaceus, this potent triad has been shown to decrease glucose absorption and circulating blood glucose. According to a number of animal studies, bitter melon has also been shown to reduce insulin resistance and protect against diet-induced hyperglycemia and hyperinsulinemia. For this, I simply take two capsules of Kion Lean before or after my largest or most carb-heavy meal of the day.
5. Berberine – Dihydroberberine, berberine's more biologically available derivative, has been shown to inhibit mitochondrial respiratory complex I, a mechanism for the action of berberine to activate AMP-activated protein kinase and improve insulin action. Berberine has also been shown to significantly lower fasting blood glucose, hemoglobin A(1c), triglyceride, and insulin levels in type 2 diabetics by increasing insulin receptor expression. It also improved liver function. Another study found that 500 mg of berberine taken twice per day by patients with type 2 diabetes lowered blood glucose, fasting insulin, and blood lipid levels.
For more information on all of these compounds, read my article “5 Simple Steps You Can Take To Live Longer, Banish Blood Sugar Swings & Massively Enhance Energy Levels.”
For my recent podcast guest Josh Clemente, consistent exercise and sleep are the two biggest factors for managing his glucose levels. For me, it happens to be cold thermogenesis and weight training. My point is, what works for one person to manage blood glucose may not necessarily work for someone else. The best way to determine whether something works for you is to check your glucose levels, which you'll learn how to do below.
Summary
A CGM is one of the first bio-wearable devices that can give you real-time feedback into the complex processes happening within your body when you create and burn energy. These metabolic systems touch every cell in your body, so they have effects felt far beyond just the post-meal response.
To recap…
- Many people wearing a CGM are surprised by how much sleep affects their glucose responses. Research shows that too little sleep, too much sleep, and poor-quality sleep can all cause acute insulin resistance.
- Chronic stress is a sneakier metabolic foe as we often don’t realize it’s happening and may blame poor glucose levels on other factors. But, stress hormones have real effects on your ability to maintain healthy glucose levels.
- Exercise is massively beneficial to metabolic health, whether it's a HIIT workout or just a walk after a meal. Any activity is better than no activity in bringing glucose levels down.
- The good news about alcohol and glucose is that moderate drinking doesn’t seem to affect your blood sugar and may even help your long-term metabolic health. Just be careful you don’t go hypoglycemic if you’re fasting or ketogenic.
- Nutrition, of course, has probably the greatest effect on your metabolic health. By aiming for a diet that minimizes blood sugar spikes, you can put your body in the best position to burn fat, as well as stave off destructive insulin resistance.
Observing the interplay between diet and lifestyle factors such as getting enough sleep or managing stress can give you invaluable, actionable insight into your own body’s workings and help you make informed decisions regarding your health.
So, you're probably wondering by now. If you're not diabetic, how can you get a CGM?
While CGMs were initially designed for those with certain medical conditions, and are only available through prescription, they are becoming increasingly popular as wellness tools. Levels Health uses a telemedicine network of doctors to bring CGMs to the masses by prescribing members two continuous glucose monitoring devices to be used for a 28-day monitoring period. Paired with their app—which interprets your data for you, scores your meal and lifestyle choices, and allows you to run experiments across different inputs such as diet and exercise and recovery techniques such as temperature therapy—just about anyone can have real-time access to their glucose levels.
Levels typically has a pretty hefty waitlist, but you can skip the line when you use my link.
To learn more about Levels Health, listen to my podcast “A Rocket Scientist Homeschooler's Insider Blood Glucose Monitoring Secrets, The Best Way To Use A Continuous Glucose Monitor (CGM), Blood Sugar Biohacking Tips & Much More!” with founder Josh Clemente.
How about you? Have you ever tracked your glucose with a continuous glucose monitoring device? What interesting information did you glean from it, or what sorts of trends did you see? Leave your thoughts, comments, and questions below.












Incredibly detailed information. Never heard of using a CGM for so many different conditions. Thank you!
Ben, Which CGM devices do you recommend? Currently using?
Thank you . I really enjoy your podcast and kion products,
Dave V
Ben – are there levels that can be deemed too low, fasting state or otherwise? I recently had blood work with glucose levels of 59..I wasn’t fasting but I hadn’t eaten a lot that day/ had worked out a bit earlier prior.
I’d love to hear your take on gestational diabetes diagnosis, and the effects of age. Apparently there are two different standards to diagnose GDM. Under the National Diabetes Data Group standard, I’m not at all. But under the Carpenter-Couston standard, I was 3 points from a failing diagnosis! So a GDM diagnosis depends on what your state adopts.
It is shocking what kind of a glucose spike I get should I eat a bowl of cornflakes😱
My 4am waking and hot flashes (male) correlated to low blood sugar (54).
Also I have “dawn effect” where my blood sugar rises to meet daily activity, when the sun comes up, though I have not eaten anything for many hours and I am still dozing. I never would have figured this out without a GCM. My Father worked out the biochemistry for the sensor in the 70’s. It is disappointing that it took so many decades to show up in beneficial device!
Good stuff. I did my own 14 day CGM experiment with Veristable (Finnish company), it can be read here: https://ilmostromberg.com/14-days-of-continuous-blood-sugar-monitoring/
Would be interesting to try out levels health also
Just today I tarted today wearing a CGM! I am not diabetic but I love Bio Hacking. I slept really well last night (my Oura ring said 2.5hrs Deep and 1,5hrs REM) but I felt so tired today. My CGM reading was around 4. I fasted for 14 hours broke it with a black.coffe. I had two slices of the Life Changing Bread with almond butter. For lunch I had salmon and rice with vegetables. I felt so tired after lunch I had to lie down. When I woke an hour later feeling even kore tired my CGM reading was 3.2! What is going on?! I ate some fruit and that got it back to 4. Fascinated by these results but have no idea what it means. Looking forward to seeing what the results are the next 14 days.
I’m wearing my second CGM. One night I had a very stressful Sleep. The evening before I’d eaten dates, dark chocolate (70%) and nuts. There were two spikes during the night. Last night I fasted in the evening. Sleep was fairly disturbed. I had two dips of glucose. Now I have something to eat in the evening so my glucose doesn’t spike or dip during the night.
How do you know what your glucose levels are doing in the night? Does your monitor track that? Which one do you have?
I have a Freestyle Libre. It’s about £54 and for two weeks. It’s a small round sensor with sharp edges. I had to get a box of large cgm sticky plasters that cover the sensor.
It does monitor my glucose level during the night.
I wish they would last longer and monitor other things; like Ketones and Cortisol.