December 21, 2015
In last week's article “Four New, Cutting-Edge Ways To Easily Shift Your Body Into Fat-Burning Mode & Ketosis“, I finished with a somewhat mysterious word of caution to those who consume oodles of coconut oil (or MCT oil, for that matter).
Mystery, begone.
In today's article, myself and my friend Alyssa Siefert, PhD (a Biomedical Engineering Instructor/Researcher at Yale) are going to tell you about the dark side of coconut oil, and reveal a cautionary, scientifically accurate tale for any coconut oil extremists who insist on adding oodles of coconut oil to every smoothie and spoonful after spoonsful of MCT oil to every cup of coffee.
So go ahead, slowly step away from the giant vat of coconutty goodness, and open your mind to the possibility that, in the same way that too much protein could reduce lifespan and too few carbohydrates can cause joint and gut damage, too much coconut oil and MCT could also be a bit rough on your body…especially if you fall into the specific categories we discuss in this article.
——————–
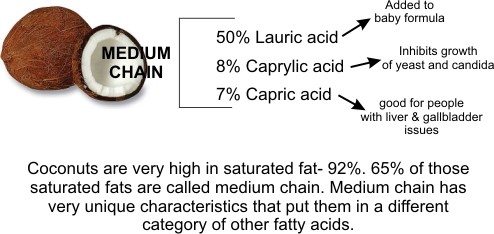
If you've recently looked into topics like ketosis, fat burning efficiency, low carb diets, or even candida cleansing, you've no doubt heard of the myriad of benefits derived from coconut oil. Because it is rich in the medium- and long-chain fatty acids (MCFAs and LCFAs) you're about to discover, coconut oil has too many compelling medicinal, metabolic, and cosmetic uses to list here.
And let's not beat around the bush: you'll find extra virgin coconut oil, full fat, non-BPA coconut milk, MCT oil and other similar fats recommended quite frequently here at BenGreenfieldFitness.com
However, the recent paper “Dietary Fatty Acids Directly Impact Central Nervous System Autoimmunity via the Small Intestine” shed light on the potential downside of medium- and long-chain fatty acids (MCFAs and LCFAs).
This well-designed, high-impact scientific paper showed that lauric acid (LA), which usually makes up 50% or more of coconut oil, tips the balance of T-cells (immune cells that actively participate in the immune response) towards the production of inflammation, and also, in mouse models, exacerbates multiple sclerosis (MS), in which your immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body.
So should people with intestinal inflammation or risk of MS go against the popular opinion of the internets and the majority of new diet books out there and instead limit their consumption of coconut and MCT oil?Can too much coconut or MCT cause inflammatory or immune issues in your body?
Can too much coconut or MCT oil cause inflammatory or immune issues in your body?
Let's make some logical, data-driven conclusions, shall we?
————————-
First of all, what are MCFAs, LCFAs, MCT, PUFAs, MUFAs, and all these other confusing alphabet letter soup phrases?
Fatty Acids (FAs) are simply molecules consisting of long hydrocarbon chains capped with a carboxylic acid (COOH). This carboxylic acid is where “acid” part of fatty acid comes from. Fatty acids are termed “saturated” if there are hydrogen atoms at every possible position on the carbon chain, and “unsaturated” if there are open positions for hydrogens on carbons that are instead filled by a double bond between the carbon atoms.
Here's a pretty picture to demonstrate:
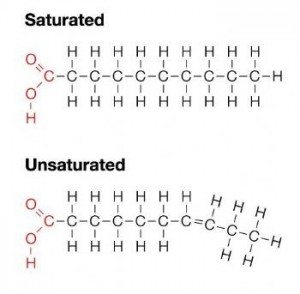
FAs that only have one double bond are called mono-unsaturated fatty acids (MUFAs), while FAs with multiple double bonds are polyunsaturated FA (PUFAs). Fats are formed by chains of fatty acids connected together with glycerol, and are classified as monoglycerides (one FA per glycerol), diglycerides (two FA per glycerol), or triglycerides (you guessed it – three FA per glycerol). If this is getting too nerdy to remember, just think that saturated fats are solid at room temperature and unsaturated fats are liquid at room temp and often used as cooking oils.
Fats, like those you would consume from foods, are formed by chains of these fatty acids that have been connected together with glycerol, and these fats can be classified as monoglycerides (one FA per glycerol), diglycerides (two FA per glycerol), or triglycerides (you guessed it – three FA per glycerol).
If this is getting too nerdy to understand, just remember: saturated fats are solid at room temperature (like coconut oil) and unsaturated fats are liquid at room temp (like extra virgin olive oil).
Anyhoo…let's get to know these FAs even better…
…Short-Chain Fatty Acids (SCFAs) have one to six carbon atoms, including acetic acid (C2), propionic acid (C3) and butyric acid (C6). SCFAs are made by the fermentation of dietary fiber such as vegetables by your intestinal bacteria (AKA your microbiota) and these SCFAs exhibit numerous health benefits, especially for preventing metabolic disorders by turning white adipose tissue into brown adipose tissue and by regulating blood sugar. SCFA treatments have also been shown to ameliorate mouse models of intestinal bowel disease (IBD) and allergic asthma.
Then we have FAs with longer chains of carbon atoms. The famous MCT oil is composed of Medium Chain Triglycerides that have FA chains ranging from 6-12 Carbons, including caproic acid (C6), caprylic acid (C8), capric acid (C10), and lauric acid (C12) – though, as you learned about in last week's article about how to get into ketosis, it is hotly debated among nerds whether lauric acid is considered a MCT or LCT.
And yes, FAs get even longer. LCFAs have 12 or more carbon atoms and include eicosapentaenoic acid (EPA) (20 Carbons), docosahexaenoic acid (DHA) (22 Carbons), and, depending on whom you ask, lauric acid (12 Carbons).
OK, enough with the science lesson – when it comes to stuffing or not stuffing your face with coconut oil, why does this stuff even matter?
—————————–
To answer this question, let's get back to that recent study on coconut oil mentioned earlier.
While numerous internet articles on many popular diet and nutrition websites make a claim that over 1500 peer-reviewed scientific studies confirm that coconut oil is healthy, a quick Pubmed search shows that although there are that many studies relevant to coconut oil, many of them are not actually saying that coconut oil is a panacea.
Take a look at the screenshot below to judge for yourself.

Sure, there is indeed a great deal of high-quality scientific research showing that coconut oil has many health benefits, and even health benefits beyond the ones you've probably heard about a million times from various health gurus.
For example, did you know that coconut oil can mitigate the damaging effects of antibiotics? In this study, Nigerian researchers gave rats a broad-spectrum antibiotic (Trimethoprim-sulfamethoxazole), and produced significant increases in liver toxicity markers like serum total bilirubin, lactate dehydrogenase, and alkaline phosphatase. But supplementing these antibiotics with virgin coconut oil protected against this liver toxicity (here are a few other creative ways to limit the damage from antibiotics).
That said, the recent research findings mentioned earlier suggest that coconut oil is not healthy in all situations.
In the October 2015 issue of Immunity, a leading primary research immunology journal, the effects of FAs were meticulously investigated in a report entitled “Dietary Fatty Acids Directly Impact Central Nervous System Autoimmunity via the Small Intestine”. Download it here if you'd like.
In this study, researchers first added FAs ranging from C4 to C12 (from butyric acid to lauric acid) to naïve mouse T cells, showing that as the length of hydrocarbon backbone increased, the number of T cells that differentiated into Th17 cells increased in a strikingly linear fashion:
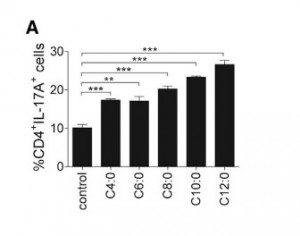
In this figure, naïve T cells were dosed with C4:0 = butyric acid, C6:0 = caproic acid, C8:0 = caprylic acid, C10:0 = capric acid, and C12:0 = LA, and the number of Th17 cells, marked by surface protein CD4 and production of IL-17, were quantified.
So what are Th17 cells, and why should we care?
Imbalanced T cell subsets drive numerous autoimmune diseases, and an abundance Th17 cells (called Th17-skewed immune system) can result in inflammatory autoimmune disease, including intestinal bowel disorder (IBD) and multiple sclerosis (MS).
See, Th17 cells are meant to attack parasites and pathogenic bacteria, but having too many of them in your body can increase the chances of their attacking your own tissues, such as myelin sheaths in the case of MS. But while Th17 cells promote inflammation, they can be balanced by anti-inflammatory regulatory T cells (Tregs), and it is the ratio of pro- and anti-inflammatory T cells, not the absolute number of each cell type, that is predictive of health and disease.
Therefore, researchers next quantified the effects of hydrocarbon chain length on Treg differentiation, finding that shorter chain FAs induced Tregs:
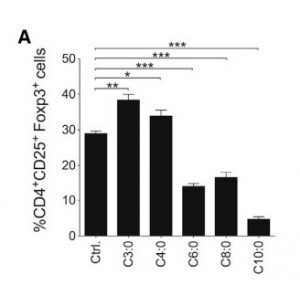
In this figure, naïve T cells were dosed with C4:0 = butyric acid, C6:0 = caproic acid, C8:0 = caprylic acid, C10:0 = capric acid and the number of Tregs, marked by surface proteins CD4 and CD25 and expression of transcription factor Foxp3, were quantified.
To determine if the Th17-skewing effects of LA were relevant to autoimmune diseases, mice with the mouse-version of MS (called EAE) were fed a diet of 30.9% fat with 13.5% of it LA (compared to control diet of 4.2% fat).
To relate this dietary regime to humans, for a person eating 2500 calories a day, that’s 750 calories from fat, and 101 calories from LA. Siince coconut oil is 120 calories per tablespoon, half of which come from LA, this translates to about 2 TB of coconut oil per day – a pretty reasonable dose. So since the dosing in this paper checks out, you can regard its results as likely relevant to your life (as opposed to studies that give crazy, otherworldly high doses of tested compounds).
Anyways, so back to this study. Mice eating higher amounts of LA exhibited Th17-skewing in the intestines, worsened MS symptoms, and changes in the microbiome (reduction in Prevotellaceae and S24-7 of the bacteria Bacteroidetes phylum). Disease worsening was actually worsened by this microbiota shift, as repeating this study with germ-free mice (that have no intestinal microbiota) did not result in Th17-skewing.
To be clear, these results show that high amounts of coconut oil can create rampant inflammation, nerve damage and worsen an autoimmune disease.
But wait, there's good news.
Remarkably, feeding mice the SCFA proprionic acid (C3) both prevented the onset and alleviated symptoms of MS. The overall conclusion of this study is that through the intestinal microbiota, LCFA can induce pro-inflammatory T cells, and SCFA ca induce anti-inflammatory, regulatory T cells.
Therefore, SCFA can mitigate the harmful effects of LCFA.
In other words, if you consume SCFA along with your coconut and MCT oil based LCFAs, you mitigate the damage.
And where do you get SCFAs in quite generous amounts?
You guess it: vegetables.
A high-fat diet? Thumbs mostly down.
A high-fat diet mixed with a high intake of nutrient-rich, SCFA-inducing plants? Thumbs up.
Again and again, we see that health is achieved through balance (and at the end of this article, we'll give you a link to a podcast in which I discuss the details of a high-fat, plant-based diet).
—————————-
But wait. The tale of the dark side of coconut oil is not quite finished.
Another recent study highlights another potential risk of coconut oil. Researchers investigating the effects of soybean oil, alone and in conjunction with fructose (which has increased significantly in American diets), fed mice 40% of their daily calories from fat, either from coconut oil alone or a 50/50 mix of coconut and soybean oils.
Compared to 40% of calories from coconut oil alone, mice consuming soybean oil had increased obesity, insulin resistance, diabetes, and fatty livers, showing that the adverse effects were from the chemical nature of soybean oil, not the macronutrient breakdown.
So that’s a win for coconut oil, right?
Maybe not.
Interestingly, in the same study, mice fed all high-fat diets tested (coconut oil, coconut oil + soybean oil, with and without fructose supplementation), exhibited significantly reduced lengths of both small and large intestines. Researchers reasoned that this intestinal shortening, which has broad implications for microbial colonization and nutrient absorption, is likely due to reduced fiber intake, since 40% of calories were fat.
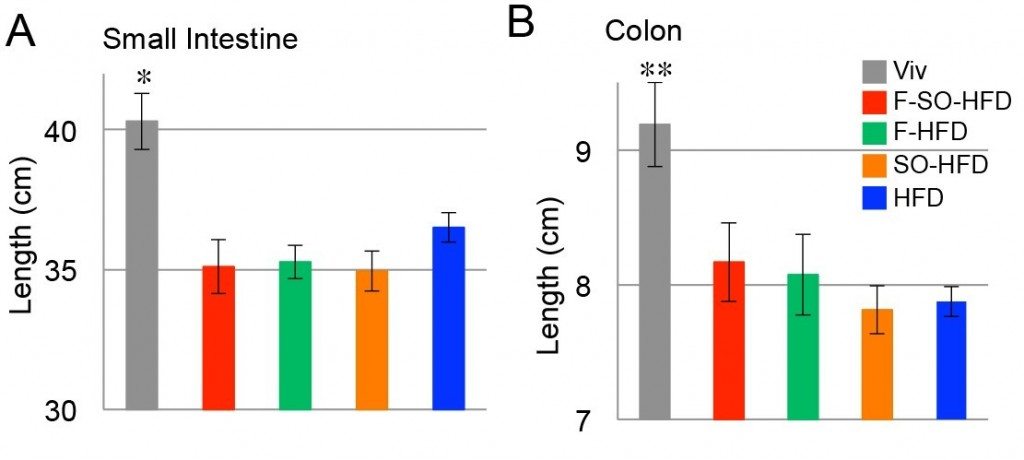
Lengths of small intestine (A) and colon (B) of male mice on the indicated diets for 35 weeks.
OK, these findings are kind of scary – so now should I stop eating coconut oil?
Nope.
Back it up.
Coconut oil + SFCAs = good.
Coconut oil + fiber = good.
Coconut oil dumped into a cup of coffee, followed with a lone carrot beside your lunch and perhaps a scant serving of roasted vegetables with dinner? Not so good.
To put this in perspective, as you can read about here, Ben eats about 15-20+ servings of plants per day. And because of this, he gets away with a decent amount of coconut milk, coconut oil and MCT oil intake. All the SFCAs and fiber help balance out the potentially damaging effects of the fat, while still allowing him to get all the benefits of the fat.
Coconut oil, with around 90% of calories from saturated fat, 65% of which are MCTs, has been lauded as an ideal fat for cooking, ketosis, and prevention of metabolic and cardiovascular diseases. So we're not saying coconut oil is unhealthy – just that it may be overhyped, and is too often recommended without simultaneous recommendations to eat your friggin' vegetables.
As you can see, Ben likes to eat plants.
——————————
Before finishing up with a couple more practical recommendations and resources for you, here are a few caveats.
While it is tempting to accept as fact all conclusions drawn from studies published in peer-reviewed journals, as an academic, you need to realize that not all peer-reviewed journals are created equal. Scientific and medical journals are ranked by impact factor, with higher impact factors usually correlating with more rigorous, unbiased review processes of submitted data. Therefore, researchers regard conclusions from publications in high impact-factor journals, like Nature or New England Journal of Medicine, with greater levels of confidence than publications from low impact journals, which can suffer from shady and nepotistic publishing practices.
In addition, data and conclusions are only as valid and applicable as the experimental and statistical methods used. Often, gold-standard findings are found in meta-analyses, in which unbiased researchers (like epidemiologists or statisticians) re-analyze massive data sets from multiple studies. Still, when considering whether or not to apply findings from health-related studies to your own life, think about how robust the methods used are (did the researchers study 10 people or 10 thousand?), the dosing regime, and how similar you are to the experimental subjects.
Why are we telling you this?
Because the studies you just learned about are indeed valid, applicable and gold-standard studies. Not N=1 experimentation or tiny or sponsored by the anti-coconut-oil industry. So they're important for you to know about.
But wait…weren't these studies done in mice guts? Last I checked, we didn't have tiny tails and cute whiskers…
The recent scientific paper “How informative is the mouse for human gut microbiota research?” helps elucidate this for us (the whole paper is actually quite fascinating and worth a read, especially if you don't have a social life):
“…their advantages are numerous and, furthermore, the amount of research and knowledge on mouse gastroenterology, genetics and immunology far surpasses any other model. Murine mouse models provide a range of customizable genotypes and phenotypes far superior to any other model organism. They have thus played a very important role in the emerging gut microbiota research field. Owing to their widespread use in biomedical research, these models are complemented with extensive knowledge on genetic background and deep phenotypic and functional characterization. Moreover, with well-set-up standardized mouse house facilities throughout labs in the world, conducting experiments on mouse models, even germ-free ones, can be more easily achieved than with other models.”
Finally, as pointed out at the WholeHealthSource website, “Butyrate Suppresses Inflammation in the Gut and Other Tissues”:
“There are two main ways to get butyrate and other short-chain fatty acids. The first is to eat fiber and let your intestinal bacteria do the rest. Whole plant foods such as sweet potatoes, properly prepared whole grains, beans, vegetables, fruit and nuts are good sources of fiber. Refined foods such as white flour, white rice and sugar are very low in fiber. Clinical trials have shown that increasing dietary fiber increases butyrate production, and decreasing fiber decreases it.
Butyrate also occurs in significant amounts in food. What foods contain butyrate? Hmm, I wonder where the name BUTYR-ate came from? Butter perhaps?”
So yes, although you can overdo butter just like you can overdo coconut and MCT oil, if you are indeed consuming lots of LCFAs and MCTs, consume a bit of butter too. Thank you, Dave Asprey and Bulletproof Coffee, for pointing that out quite extensively.
——————————
Anyways, back to those practical recommendations.
Dr. Alyssa Siefert has a tablespoon of unrefined (virgin) coconut oil in her morning coffee, but she is mindful not to exceed a few tablespoons a day unless she is matching this increased LCFA consumption with fiber from whole plant foods, as fiber intake directly correlates with SCFA production in a healthy gut. She also reads labels to ensure she's consuming organic unrefined (virgin) coconut oil that hasn't been hydrogenated.
And, as mentioned earlier, Ben accompanies his 70-90% fat based diet with oodles and oodles of plant matter at each meal, and doesn't count any carbohydrates he gets from sources like kale, spinach, tomatoes, etc. as part of his total daily carbohydrate intake.
The adverse effects of a high-fat diet may not result from what you're putting in your body, but what you're taking out (usually fiber) to allow increased intake of fats like coconut oil.
If you do happen to be a person whose baseline immunity tends toward inflammatory (for instance, a history of autoimmunity or skin conditions), then you should be especially be cautious about the amount of LCFA, MCT's and coconut oil you consume, but we still consider coconut oil a much healthier replacement for the unsaturated fats like canola oil (that used to be touted as heart-healthy, especially for cooking).
So don't fall into nutrition extremism. Including some coconut and MCT oil in your life is great, more is not necessarily better, especially if you're not going out of your way to eat plants, which can be admittedly more time-consuming than spooning fat into a cup of coffee or tea.
Finally, here is a link to a podcast Ben recorded with Dr. Terry Wahl's, in which they discuss exactly how to eat a plant-rich, high-fat diet.
——————————
If you enjoyed this article and want more balanced, accessible science updates on your newsfeed, then check out Dr. Alyssa Siefert at The Sociable Scientist on Facebook! And leave your questions, comments and feedback below. And eat your vegetables.


Thank you for this article! I switched from butter to coconut oil and have been experiencing major muscle/joint pains, brain fog, memory issues, kidney stones, herniated disc in my neck. I’m wondering if the coconut oil is the culprit. I switched from butter as I have endometriosis and discovered through PubMed and experimenting that cream is very estrogenic and causes endo flare ups. I will eliminate the coconut oil and see what happens. I’m 49 and have been feeling 100 y.o. due to joint and muscle pain. Also, I have a chronically high WBC on blood tests. I wonder if the coconut oil can cause that? There is no infection and doc is confused by the constant elevation. Trying to heal from the disc issue and inflammation causes pain. Thanks!
I started substituting 2 table spoons of olive oil with 2 table spoons of coconut oil in my 1800 calorie per day meal plan. Nothing else was changed. Within one month I started having intense joint pain in both thumbs. So, I switched back to olive oil. It took about two weeks before the pain started going away and about a month to completely go away.
I talked to my doctor about the problem and she had never heard of any problems with coconut oil.
Have anyone else had problem with coconut oil?
Hi W. Reid
I started Coconut oil and get a lot of bloating and leg joint paint and lower back pain… After a few tests Coconut and Oil came up as a positive for intolerance.
Most people I talk to have no idea that scalp therapy shampoos for fast hair growth (of course with no sulfates, no parabens, no DEA) are a thing. Individuals are now able to attain longer hair and attain more options. Definitely worth investigating.
Whether you’re going over hair loss, damaged hair, avoiding hair disorders, hair growth, hair health more often than not, the same thoughts apply.
As a rule of thumb, you want to stay away from hair products and treatments that include chemicals like parabens, DEA or sulfates.
What is healthy for your hair is good for your skin all the same.
Clearly your content above hits the nail in the head for so many reasons. It stays away from the usual errors and mistakes too many fall into: utilizing ineffective alternatives. Keep up the great content!
View the Best Movie of All Time
What video do you want to be able to watch today?
Sniper films may be required on your list. This will be
the most exciting shooting struggle, where every sniper actions
is always interesting to be able to watch.
I sell vegan dishwashing soap made with 100% coconut oil. All soaps high in coconut oil have caused extreme dry skin for me over the years, so I do not personally use them. I know many people who have no problem at all with coconut oil soaps. I have started to have joint pain and stiffness (about a 7 out of 10) in my hands and wrists whenever I have to test my soaps by washing my hands with them! (Star9Divine.com)
Some people however pay so much money at one time to lift the likelihood of winning.
The system where betting money is through your financial institution is secure to work with, and the transaction is
always between your account and the Ladbrokes.
Simple system described in steps. Many are easy individuals
simply struggling to get by. This information supplies all the information it’s essential to get
into the sport. But the thing is that to extend your possibilities of successful, you
want to place a bet day-after-day. As a substitute, you’ll be able to get all the data
you need from that very same site. As lengthy because the owner of the Bitcoin looks after it correctly utilizing a excessive-security wallet and two-issue authentication, will probably
be extremely troublesome for anyone else to get entry to their funds.
At any point, nonetheless, the bookie can soar in and make adjustments to
the strains that can be found to his players if knows he
will likely be getting heavy one sided action.
If you are one of those individuals who doesnt like cats, Im sorry to listen to that.
For the above instance, it could seem like -7.5 (-110).
Other players can legally purchase Mega Hundreds of thousands Lottery tickets on-line by the lottery agent you see mentioned above.
As an illustration, MEGA Hundreds of thousands is a multi-state lottery and it operates in eleven states.
For example, you wouldn’t need to select simply any race horse in hopes of
profitable a wager. 5. Bet on sports activities by putting your wager.
When you click on the sport of your choosing make sure to
bookmark the web page so you’ll always have probably the most current and up to date sports betting odds at
your disposal. In this method, chances are you’ll choose a low number from the given set corresponding to 1-50 like 1.
Some winning numbers have two consecutive numerals, though not on a regular
basis. After which with the time you saved do one thing more productive than you’d
have completed appearing like a poor particular person.
Aside from coconut oil, this assessment could be applied to any long-chain fatty acid, such as EPA and DHA found in fish oil. Maybe the fish oil supplements, separated from the fish, can cause this imbalance of the T cells and Tregs causing inflammation.
Dear Ben – as always – your rock. This article was super helpful. I fit squarely in the coconut in coffee and not enough veggies group – I’ve been using Laird Superfood Creamer… daily for the past 6 months… and found myself in the past few weeks past the tipping point with a series of infections and systemic inflammation (tendonitis seemingly in all major tendons and super sensitive to acupuncture.) Now I know Why (I had been thinking about what I had been doing differently and realized it was the creamer). And I can also confirm that I over 50 and have skin sensitivities – and so am at greater risk. You have validated my hunch I needed much more veggies and fiber and inspired me to “do the right thing.” I am also investigating and implementing how else I can reduce all this inflammation, and bring my microbiome and rest of body back into homeostasis.
In thinking of the use of coconut, first consider the peoples in the tropics who use this fruit everyday. If coconut was that bad for you, the tropical peoples would be dropping like flies. But strangely, that does not happen. The trouble with new arrivals to the use of coconut is that, they have refined palates to begin with and they just want the oil, which frankly is simpler to use than the whole nut. But remember for every poison, nature provides the antidote. In the case of coconut, the poison is entwined with its antidote. Much like a whole orange versus its juice. Separate them and they become slow killers no matter the rave.
This is a powerful statement to me: “But remember for every poison, nature provides the antidote.” A perspective i don’t think everyone would agree with but I currently do
Consuming Coconut can be good, but extracting the oils and processing them isn’t :)
Thank you for this article. I’ve been taking coconut oil softgels for about 3 years. It helped me greatly with a sudden bout of hives, in addition to a low histamine diet. I never would have linked this to possibly making autoimmune conditions worse. I also have scalp psoriasis and occasionally have eczema. Recently, I began dry brushing to help detox my lymphatic system which helped with my eczema flare up. I did this daily for 2 months and it worked wonderfully, until it didn’t. I read many articles on dry brushing and very few said anything about avoiding it if you have eczema. It turned out that dry brushing just drove my already over active immune system into overdrive. My body acted like it was allergic to everything…certain foods, skin care products, you name it, caused itching and redness. My sleep patterns were all off. It was as if my body was in a constant state of inflammation. I stopped dry brushing, but the effects were still plaguing me. Then, I saw this article. Today was the first day I stopped taking coconut oil, and what a difference. The itching stopped and my level of pain has greatly been diminished. I know it’s only one day, but I am cautiously optimistic. I feel SO much better! I must just be one of those people who is sensitive to it. Thanks again!
It sounds like you have gluten sensitivity, wheat, oats, corn, peas, dairy, rice are just a few villains with gluten, or proteins very similar to gluten in how they are perceived by the body. No grain, no pain book.
Does it make sense to actually eat a chunk of coconut in order to add MCT to your diet ?
instead of separating out the oil from its natural fiber
read your article on Coconut oil and want to say thank you. You may think this is not really appropriate for me but I started the Keto diet not for weight loss or muscle building but for COPD and asthma, about six weeks ago. My lungs improved and I can’t tell you how good it felt. However, suddenly I became almost rigid with arthritis and got a recurrence of an old stomach ulcer. I’m 68 and female. I realised it could be the coconut oil and along with your article and the following posts felt sure it was. Now I need to research the alternatives to coconut oil, maybe virgin olive oil however just read a poor report on conola oil. So the quest goes on. I read “How I reversed my Moms COPD” a book that sort of spelled out a diet similar to Keto without mentioning it and I began to realise basically it was. I can’t tell you how well I’ve been but took up the Keto as a better guide. Apart from this bugger off a hiccup it’s been great as though I was getting my life back.
Yours
Christine Weepers
Christine Weepers, try the Paddison Program for Rheumatoid Arthritis. Lots of videos on Youtube and Pinterest has a few posts with the elimination diet and the guide for rheumatologists. It works. It’s hard work and takes patience, but it works.
Woah
..great info…info…ugh…nutrition is so complicated these days.
I was taking so much monolaurin to get rid of an ebv virus that reactivated. After taking so much my hair started falling out and they can’t find the reason why. I’m so fatigued all the time I just want my life back and I’m only 23. Now I deal with so many chronic fatigue problems. If any help please let me know. I can’t take it anymore. After all of this I don’t even get nervous anymore I used to be a really nervous person and now nothing I don’t know what this means.
Have you got amalgam (metal) fillings in your teeth?
Hi Tiffany,
I have an autoimmune disease and so does my 13-yr old daughter. What you are describing sounds suspicious to me and I think of autoimmune or adrenal insufficiency issues, which are common in young women in the US. Functional Medicine practitioners have long linked these medical problems to the standard american diet of processed junk food. Have your PCP do a thorough blood work-up to try to identify what’s going on. Also, I want to give you some positive news: I have been able to control my autoimmune issues quite well with diet: I use a Paleo/anti-inflammatory hybrid that works for me. I have a good friend with MS and she has been able to do the same through diet and exercise – her disease has been in remission for many years.
If you find out what is making you feel lousy, you might want to try addressing it with a functional medicine specialist and possibly diet and lifestyle changes. Wishing you good health!
Can I ask you how were you taking? I just started with 600mg. thanks
I have m.e and ms. The only thing that seriously stops anxiety for me is when my MS gets worse. I would say you’ve got MS, and maybe the monolaurin made it worse. Lauric acid makes ms worse, which is similar to monolaurin.
It could be histamine intolerance, worth looking into.
There are so many food intolerances , it’s a job working through them but can make a big difference to the quality of life. Good luck!
Hi Ben,
I’ve been struggling with Alopecia Areata (Autoimmune issue) for a little over a year now, and it started after 2 consecutive bouts of food poisoning -I’ve been on the bulletproof coffee (2 tbsp Caprylic Acid brain octane oil + 2tbsp Grass-fed ghee) for about 2 years.
After doing lots of research and trying to figure out how to beat AA I decided to go on a Ketogenic diet and also started consuming probiotic, digestive enzymes, glutathione, l-glutamine, turmeric and increased my vitamin d consumption all to try and heal the leaky gut which Is likely the cause of the AA.
I don’t consume a huge amount of coconut oil but obviously have a BP coffee 5 days a week and sometimes use the brain octane oil throughout the day to increase my fat consumption – Do you think eliminating the brain octane oil from my diet would help? or alternatively is there anything you recommend I supplement with the bulletproof coffee to counteract the effects?
Really appreciate any response you are able to provide.
For this sort of thing, I'd need to gather much more information about you via a personal one-on-one consult. You can sign up for that at BenGreenfieldFitness.com/coaching
Day 1 of taking coconut oil my brain said take more but my joint pain was starting to return. It happens sometimes so I ignored it. Day 2 of coconut oil I spent the day trying to counter sinus inflammation and supper resulted in too much of a flare up to finish eating. I spent the night snacking on things I knew would not increase the irritation. I still had a craving for coconut oil. Day 3 I ran out of meal replacement shakes and was planning to grab some yogurt when I realized I had to leave for an appointment. I drank my coconut oil filled tea and didn’t get food for a few hours. It started with abdominal bloating and moved on to “I’m dying”. By evening all the signs of inflammation are back. My joints hurt, my head is foggy, I’m tired, it’s hard to breathe, the sinus pressure goes to my ears, my abdomen is bloated, my bladder is definitely inflamed, I want to stand in an ice cold shower even if I’m cold, and I took my laptop to bed to figure out why it feels like all my months of steadily reducing inflammation and improving digestive function are gone. It will take a few days of stopping/reducing it to truly tell but I’m quite certain with where problems started and the timing it all lies with the coconut oil. The thought of taking any more of it today also shifted to nauseating.
Along with other sources I came across this all makes sense to me. So take less coconut oil and not on an empty stomach…. In the meantime I wonder if I have any quick fiber/carb sources left on hand in the house after my integrative health doctor has been pushing me to eat more protein and fats.
I made a mistake to fry pork on coconut oil and olive oil and a had an attack of gout. Several days later I am still suffering.now I am on lemon juice vegetables and never coconut oil again.
Maybe it was the pork and not tbe coconut oil that caused it. I’ve read good reports on coconut oil and gout.
Look it up
I thought I was going crazy but I am experiencing similar issues. I thought I was doing my body good by adding coconut oil multiple cups of coffee. I had stopped using the oil for about a month and was focusing on increased hydration. During that time, my joint pain and swelling decreased greatly. Two days ago, the only change was adding back the coconut oil and the joint pain and inflamation is back full blown.
Eat large quantities of fresh, raw veggies. Don’t use any processed foods. Just throw a variety of greens, carrots, onions, etc. in a huge bowl and eat it all. Eat baked or nuked sweet potatoes for calories with fresh, raw ginger. Stick with that and lots of water and vigorous exercise and your inflammation will likely subside quickly. I wouldn’t add the oil back until go without inflammation for at least a month. Then, keep it minimal.
Great information and thanks! :) I have always been a bit “cautious” around coconut oil *whew. Just a little in my coffee with a little butter (grass fed/organic/blahblahblah).
I found this info hoping it would have mentioned COPPER and how much is tooo much with coconut oil? Don’t even LIKE the fact I have the apoe3 AND apoe4 — Alzhiemers just go away! NOW.
:)
I am glad that I found this article. I have been taking Monolaurin tablets since February to combat some candida overgrowth in my stomach which is linked to my chron’s disease. Basically using this supplement to boost my immune system. However 3 weeks into the daily regime ( started with 500mg , later 1000mg) I started to develop a bald patch at rear of my head. Small bald patches also appeared within the beard area. I visited my doctor who diagnosed alopecia areata . I have never had alopecia nor anyone in my family.
Has it grown back? sorry to hear that. hope you are ok.
Was looking up monolaurin info for obvious current antiviral issues…
Odd..and certainly very small sample size here n=1 sort of situation but I just finished a canister of monolaurin…was taking along with my usual stack for better immune/anti viral reasons…
But, before reading this or anything related, I could have sworn my hair was thinning a bit at the upper/outer part of my hairline on both sides in the front which seemed weird. I have always had a very thick full head of hair as have both of my parents..and I’m in my 40’s now. The timing is strange….
Thought it was maybe stress or some nute deficiency…but after reading your anectode, and the timing etc….curious…
What about olive oil, avocados or nuts and seeds?
Hi Ben, I notice you mention Bulletproof. Would making Bulletproof coconut oil , butter but with cocoa instead of coffee- that is my Bulletproof hot chocolate count as fibre and so not contribute to inflammation. I had read that cocoa is full of fibre a delicious food for the intestinal microbes and so would seem along with the butter to be T Cell Reg perfection. Am I correct?
It definitely helps, but also include plenty of plant matter throughout the day.
My integrative doctor recommended for me to blend 1whole coconut water including its meat with cucumber to ease pain from rheumatoid arthritis. Consequently, what I got instead ….. was worst intensive pain.
Do not listen to this bullshit. I have used virgin coconut oil with cannabis to cure cancer. Aid in controlling sugar levels; saved legs and feet and probably other limbs (can’t be sure of all it has saved) from diabetes and one with hardened arteries (high cholesterol build up in the legs. He was supposed to get them amputated but didn’t want to. Doctor sent him home to get his affairs in order and that’s when he used the oil I make I call the Tree Of Life oil. I teach for free how to make it and it’s made with just cannabis and coconut oil… leave the soy alone (GMO)!!
The reason… we don’t grow that crop…
He is alive and walking on his white (no longer black with sores) within a year. Within a few days he started itching in his legs and that was the beginning of the healing. Without coconut oil the Tree Of Life does not work at least for diabetes and pain.
Trudy Ann Stergiopoulos is my name. I am the only one in the world. If interested look me up on FB or find me at the social.treeoflifecompassionateministry.org
It’s NOT BS. Some people cannot handle Coconut oil for genetic reasons. Go read Dr Amy Yasko’s Chapter 6 book; it’s available online too. I cannot tolerate whole or coconut oil. You must have genes that can tolerate it.
I’m starting to suspect that I can’t handle coconut oil either. I have had health issues for over a decade and I think back about the time I started adding coconut oil to my diet and baam!, it’s about the same time I started having issues.
As of today, I’m going to take it completely out and no more coconut anything and see how I feel. Crosswind is correct, not every body handles foods the same way. We are all genetically different.
I am not officially at a loss. I have 2 spoons of coconut oil a day and a 400ml coconut milk with half a kg of spinach/broccoli mix in my curry.
I dont eat meat but I have a 60% high fat diet.
If I remove Coconut fat…. what fat is left! I’ll just be eating spinach and nothing else.
Hi Ben, sorry if I’m not absorbing all the more technical content of the article with the time I have today. Curious your thoughts whether coconut oil’s effect on inflammatory immune cells, contributing to autoimmune damage in the CNS, might be indirect due to a pathogen or parasite fleeing to parts of the body that do not absorb high levels of coconut-derived substances? I’m seeing more posts about treating endemic infections/invasions versus, say, digestive ones. And how these organisms may be attracted to or repelled by what we put in our digestive system, bloodstream, etc.. Thanks!
That is somewhat possible. Tough to say unless you actually test for pathogens or parasites, like this: https://greenfieldfitnesssystems.com/product/comp…
Ben, I have heard from many people with serious diseases to be cured, what do you have to say about that? and the many many studies about monolaurin? You could be more straight to the point, then going round and round, I think most people here skipped through. When people read this article all they see is “dark side of coconut oil”, a bit over the top and sensationalist to say the least. It’s not what you say but how you say it, just looking at just one side of the evidence, while many others have life-changing benefits.
It looks like the mice were fed coconut oil AND soy oil (assuming GMO)- I’d be the soy was the issue. Why was that even added?
Great input. Soy is a hormone disrupter even if not GMO. Hadn’t realised Soy oil was used also. How come this was not mentioned in the article
Because this article is about coconut oil.
Yes but def alters the accuracy of all the research you guys just did and results dreadfully!
I just wanted to comment. I started taking coconut oil Feb 3 2018 started keto diet…. Low protein, high fat. I have had cramping issues in my left foot from nerve damage during a laminectomy in my spine. I started getting these severe “electrical” type cramps in my left foot while I was sleeping…( They woke me) they were so bad! They lasted 5 minutes every time. Repeatedly 5-10 times a night I went to Drs. He did blood panel to see if I had electrolyte issues. I had none. Months went by they were getting worse. I actually started getting electrical cramps every night in both feet ( never had nerve damage in right foot. I was exhausted from no sleep. I had X-rays / MRI of spine/hips/brain. I see a nuerologist in Seattle who had done EMG other blood tests looking for a reason for electrical cramps… In the mean time 7 months later after hearing that coconut oil might not be as good as people think, then I read this article about the issue with MS and I thought maybe that relates to my nerves though I don’t have MS yes I was tested for that to. I stopped coconut oil 1 week now and haven’t had any electrical cramps. Knock on wood honestly am hoping it is the reason because the Dr was planning on giving me anti seizure medicine. Last thing I need is a drug. I’m trying to be healthy.
I wondered if there is anyone out there that had similar problem. I tell you it’s the scariest experience I have ever gone through.
Hi Britt,
YOU ARE NOT ALONE!! I have been dealing with very similar issues. Not sleeping due to cramping/restless leg syndrome (my diagnosis). Lots of pain in my joints and muscles. I just went in yesterday for an MRI of neck and hips. Also my shoulder joints are extremely painful. Then it dawned on me this morning as I was putting a huge tablespoon of coconut oil into my coffee (which I have been doing daily for about 6 months) that it could be the coconut oil. I have excluded so many other food items from my diet that can cause inflammation, with no relief. I am grateful I came across this webpage with this information. I am praying I did not do any permanent damage to myself and am looking forward to feeling better. I am a busy bee around the house, working in the yard and in my garden, but it has been extremely difficult and heartbreaking for me when I was have a very difficult time doing little things I enjoy. I will keep you in my prayers. Feel better soon! God Bless!
Great article – one caveat to keep in mind: the “gold standard” medical journals get it wrong roughly 50% of the time (the former editor of the NEJM admitted this). So i don’t place as much credence as you do, in differentiating those studies from the “less reputable” journal studies. In my experience, the less reputable studies are actually often *more* accurate than the gold standard studies.
Agreed – look at the retraction rate for journals like Nature – way higher than their subject-specific counter parts.
As a published scientist myself I was thinking just that. The shoddiest medical expertise tends to appear in the most “reputable” journals, while the most important (but commercially-career etc incorrect) discoveries struggle to get published anywhere. Also it is here suggested that those were not sponsored by the “anti-coconut oil industry”. The problem is that the whole medical research system is heavily dominated by major commercial forces, of which one of the greatest of all is the vegetable seed industry (hence the decades of “sat fat bad, efa veg oil good”). There is strong systematic bias to start projects which confirm their propaganda, and similar bias in the acceptance for publication (especially in the “top” journals), and then in support and lack of criticism thereof. Ben’s discussion here of those studies otherwise appears very competent, and it cannot be ruled out that they are indeed all sound and honest truth, but I wonder. Due to this pervasive bias and conflicts of interest it becomes arduously difficult to reach clear conclusions about just about anything health wise! But thanks to Ben for a most interesting and thorough article here.
I loved this! Thank you!
Not helpful. Way too much information. Give the corazon, then the BS. Not the library of congress with no index!!!!
Room temperature is defined as 68 to 77 degrees F. The melting point of coconut oil is 76 – 77 degrees F.
Is your site written only for people living north of the tropic of cancer?
I live in Thailand. Unless you run the air conditioner on a very high setting, coconut oil is always liquid here at “room temperature.” I wish your site and others would stop using the term “room temperature.” A very large percentage of people in this world have never seen coconut oil in a solid state.
“Room temperature is defined as 68 to 77 degrees F.”
Not round here it isn’t. When the coconut oil melts we wisely flee to Iceland or Lapland.
“Is your site written only for people living north of the tropic of cancer?”
The entire modern world was invented (by evil white supremacists) only for people living north of the tropic of cancer. Unfortunately you people down (/up?) there will have to develop your own one!
There are some other issues with the original study ttp://www.sciencedirect.com/science/article/pii/S1074761315003921 — the total fat fed to the high-fat/high-lauric-acid (LA) mice was 30.2% of the feed by weight. But if you add up the known FA breakdown of the diet, it adds up to 28.7 (including 1.5% known polyunsaturated fats by weight). So there is a “mystery” fat component of 1.5% of the feed. If these mystery fats include much trans-fat, that could be a major factor in the immune response. If these mystery fats are largely polyunsaturated, then the total PUFA in the diet could be on the order of 5-6% of total calories, and this might be enough to cause immune flare-up. Unfortunately, they did NOT study two diets that differed in only the LA content. It would have been much more helpful to compare two groups of mice fed coconut oil and butter as their fats, in varying percentages.
The article has some bad numbers in it.
The correct number is 11 tablespoons of coconut oil to get as much lauric acid as was feed to the mice. 2-3 T of coconut oil shouldn’t be a problem at all.
How to get the correct number?
If you look at the original study, it has a link to supplemental info (http://www.sciencedirect.com/science/MiamiMultiMediaURL/1-s2.0-S1074761315003921/1-s2.0-S1074761315003921-mmc1.pdf/272197/html/S1074761315003921/9195eb531ad19b39b5fe8a4504baf245/mmc1.pdf). From the supplemental info, you can get the exact diet fed to the high-fat mice: ssniff EF R/M E15116-34. There is a breakdown is available from http://www.bio-services.nl/cms/files/Groep2_lobor…
From this detail, you can see that lauric acid (LA) is 12.58% of the raw weight of the feed, that crude fat is 30.2% of the feed, and that fat is about 55% of total calories from the feed. This works out to LA providing (12.58/30.2)*55% or about 23% of total calories.
So for a 2,500 calorie-per-day human diet, you would have to eat about 23% of calories from LA. Since coconut oil is about 44% LA, and about 116 calories per tablespoon, you would have to eat 2500*0.23/(116*0.44) tablespoons of coconut oil to get this much LA. Or 11 tablespoons of coconut oil…
Okay, this is a comment about the first evidence you present, the screen shot: Five out of the six “shots” are not about coconut oil or even about fats — peanuts, sea bream, a.coli, solid waste precipitation, sponge cake, and last, MCTs which may contain info about coconut or not, I can’t really tell whether it does or doesn’t.
Relevant? Not so I would go and try to find the info. Please edit more closely.
Hi Ben,
Thank you for this very interesting article. I came across it as I was researching methods of fat absorption. I realize you were discussing ingestion of coconut oil, but I have questions about skin absorption. It has been many years since my nursing A&P classes, but I remember some of the absorption process. Simplistically, bile salts emulsify fats and chylomicrons (lipoproteins) which are only found in the intestine transport fat molecules across the intestinal wall. Our professor explained that this was the reason fats can not be absorbed through the skin. Some creams just “sit” on the skin until it is washed off, but others seem to disappear without a trace. I always thought the fat in an ointment or cream was a carrier for medication that could be absorbed by the skin. Do you know of any fats that can be absorbed by the skin and if so how is it eliminated by the body? I can’t understand why some diet plans will not allow the use of skin creams while on the diet. Do you have any insight into their dietary recommendations?
Some diet plans are very uninformed and present false information. Just look at the ever so popular Atkins diet.
Wow. I have to Avoid Coconut. I am allergic to all tree nuts and Coconut seems to give me bad reactions too, even though they say it’s “not a nut”. Coconut dried flakes and coconut OIL both increased my body temp = INFLAMMATION and Heat Flushes for me. It also gives me Brain Fog, Forgetfulness, worsens my ADHD with inability to concentrate on one thing and then i start acting OCD around the house, work, chores, shopping and trying to control other people around me, to the point family will ask WTH is wrong with me!? Even Fresh coconut is not good for me. Trust me, i have bought cases of fresh coconuts & opened them up for the water & made coconut pudding, smoothies, raw fruit pies with it. But, per Dr. Amy Yasko, some people have certain Gene Mutations that interfere with how we metabolize MCT oils like coconut and I have 1 to 2 of those genes. I tried, and it’s yummy, but I have to AVOID it.
Thanks for the article…Does that “dark side” apply to monolaurin supplement as well?
No, it is primarily the heavy amounts of saturated fats in the absence of fiber that is an issue…
It starts off saying empirical evidence show this but then the study was done in vitro.
I’ve see studies say Omega 6 oils are bad since it promotes inflammation. CLA has helped me greatly. Omega 6 oils seems big in the body building world. CLA is a natural trans fat so very healthy.
There are quite a few people who do great with coconut oil. There are some who get a negative reaction. I use coconut oil in place of industrial made oil when i have to fry something so maybe use it twice a weeks. I try to get lots of saturated fat.
You have to look at the EMPIRICAL evidence on how they worked on YOU. You have to experiment. Maybe you are some of the few who have sensitivities to coconut oils. Maybe you are taking too much of it. Experiment and adjust things accordingly.
CLA is totally different than common omega 6 fats found in veg oils. the kind in veg oils is mostly linoleic acid, where CLA is conjugated linoleic acid. It’s not the same chemical. veg oil is heavily inflammatory while CLA is a powerful anti inflammatory. It’s also a trans fat. but it’s a different chemical from the toxic trans fats in commercial oil. Empiracle evidence is great–it’s definitely important to know how you feel about the foods you’re eating, and adjust accordingly. But you won’t always feel it right away if something is bad for you. That’s one of the many reasons scientific studies like this one are so critical to our lifestyle choices.
I have a number of health issues from fatty liver to know kidney issues and joint problems and have come to think I have out of control inflammation. I never have colds and seems my immune system is too high! I have about 40 pounds of belly fat and upper abdomen fat. 53 year old male. And am on a long list of anti inflammation suppliments. Omega 3 just added a little avocado oil and high mct coconut oils at I tbl spoon and source naturals omaga 3 with all the extra 6,9 ect. Hope it helps as I was in great health till a few years ago and one after another started having these issues. Along with adrenal wired tired insomnia ( they call it the walking dead syndrome, and boy are they correct). Any thoughts just found this site this eve…
Hey John, I would start here: https://bengreenfieldfitness.com/2014/05/7-signs-… and if you want to go into detail go to https://bengreenfieldfitness.com/coachme” target=”_blank”>www.greenfieldfitnesssystems.com/ben, you'll be able to book a consult with me via Skype and we can go over everything there.
I have a question. Since fiber inhibits the absorption of fats, should the XCT oil be taken with a high fiber meal? And what is the cut off limit for fiber in a meal that would inhibit the absorption of the XCT oil?
I put it in my giant smoothie with a ton of fiber and still note lots of benefits BECAUSE those triglycerides go straight to the liver, bypassing most digestion. So this one or coconut or MCT oil are fine with fiber.
Dave Asprey describes the MCT’s capric and capryllic (XCT oil) as not even being processed by the liver at all, but simply being metabolized into ATP in very few steps (somehow). Lauric, LCT’s, and ALL other fats, must be processed by the liver. I don’t see how any of this would change the rate of absorption in the intestine though. How do those triglycerides absorb through the intestine any faster than other fats in the presence of fiber?
Because the actual processing of the fats INTO triglycerides is performed in the liver instead of in the gut.
In the study:
“For experiments under LA-rich diet, mice received a chow containing 30.9%
crude fat rich in the MCFA C12:0 (lauric acid, 13.47%), and mice on a control
diet were fed a chow with 4.2% crude fat.”
30,9% of what? Calories I guess? They don’t say. Whatever.
But more importantly, they don’t seem to mention anywhere, what the other 69,9% of the mice “chow”, was made of. Probably grains? Or worse, sugar…?
So let’s see. Increasing LA in presence of.. er… grains? Sugar? (??They don’t say??), has this and that (baaaaaaad) consequences in laboratory mice. Am I concerned? No. Are YOU concerned? You shouldn’t.
The T-cells differentiation thingy is… in VITRO.
I eat real food. My T-cells are not in a Petri dish, I’m not a mouse, I don’t eat grains, I don’t eat sugar.
I wouldn’t personally make ANY conclusion as the relevancy of this study to real-life human feeding and health. Too many plot holes in the storytelling.
Great article Ben! I always suspected coconut oil of flaring up auto immune disorder even though everyone raves about it. Can you suggest another fat to cook /fry with if you are intolerant to dairy(butter)?
Hey Ann-Marie – yep, I cover oils in detail in the first question of this transcript: https://bengreenfieldfitness.com/2009/04/episode-… Hope that helps!
I have had the same issue and suspect it might be coconut oil causing the flair up of inflammation all over my body. Going to remove coconut oil and see what happens.
THANKYOU SO MUCH!! this post has put to rest my year of uncertainty with coconut products. I have Multiple Sclerosis and am on the OMS (Overcomming Multiple Sclerosis) Recovery Program which is basically low saturated fat, plant based + sea food diet inc flaxseed oil daily, meditation, exercise and vit D. There is so much confusion on this diet as we arn’t allowed coconut products yet everyones talking about its health benefits, that now we actually need sat fat, that it’s anti inflammatory, good for MS. But the doctor who created OMS who is incredible says theirs not enough evidence – it’s so confusing for us. But this article and your interview with Dr Wahls has been fantastic. I knew that the plant based high fibre diet had to be part of it. I hope you dont mind me referencing this article on my blog!
No worries Simonne!
I have followed low carb diets before with good results. Now doing bullet coffee and fat bombs with plenty of coconut oil. All seemed good but for weeks have been fighting ear and face irritation. Corner of eyes also irritated,itchy. This is unusual. Thinking of cutting coconut oil next to see if it stops this …
This is an interesting read. I’ve been battling a rash under my left eye for the last couple months- it comes and goes. I’ve never had sensitive skin before, and I’ve avoided the doctor knowing full well they’ll give me a steroid cream and send me on my way.
I started doing some research the other day about Chinese face mapping, and the location on my face led me to believe it was intestinal (I’d been looking for an environmental factor all along).
I drink bulletproof coffee with a tablespoon of MCT oil most days.
I suspect you just added the final piece to my puzzle. Thank you.
Awesome Steve!
A Simple YES or NO would have Suffice.
Not nice at all…
No, they don’t appear to be gold standard studies.
As usual the overall diet of the mice isn’t clearly revealed.
That has much bearing on how the coconut oil would influence the body overall.
What all this basically means is eat whole coconut with fiber ?
Do these studies reveal exactly what type of coconut oil was used? This is a ‘key’ piece of information… that studies never cover. Was the coconut oil hydrogenated? This is the ‘dark’ side of research studies and the conclusions they reach.
Great observation, silver, and while neither study reveals the details of fatty acids used (I dug through the supplementary info), I am inclined to believe that the fats used were not hydrogenated because they continually cited the chemical structure as 12:0, etc (meaning that there are zero double bonds). One study pointed to an info sheet on the mouse diet used, detailed here: http://www.newcolab.com/docs/5001.pdf.
I just emailed the corresponding author to ask about the source of coconut oils, and I’ll update with info if I get it!
best,
Alyssa
The studies were not even done with coconut oil. They were done with pure fatty acids, some of which are the main constituants of coconut oil. They are specific chemical structures with exact names, they are NOT hydrogenated. hydrogenated oils would have totally different fatty acid compositions and chemical names/structures. Look at the study.
Having dropped your MCT/CO consumption down to 2T, where are you getting the bulk of your fats from then, Ben, considering you follow a high fat diet?
Olive oil, avocados & nuts?
Cheers
Jack
you name it! olive oil, coconut oil, coconut milk, avocados, seeds, nuts., etc.
Great article. I drink bulletproof coffee in the morning with 2 tbsp of caprylic acid and 2 tbsp of kerrygold butter. From what I can tell caprylic acid is not as risky as lauric acid, but it still produces a response. What kinds of foods/fiber supplements could consume to produce SCFA that would not impact my ketogenic fast?
Butyrate supplement or guar gum can work, but really ANY non-starchy plant based fibers are fine!
Thanks Ben. I’ve started drinking a celery, cucumber, kale, lemon and ginger green smoothie (with a couple of drops of stevia to take the edge off) before I drink my bulletproof coffee. I’m happy I’ve started this since it is a refreshing way to start the day.
What about organic apple pectin? Been studying and find lots of positives for supplementing wit it.
I am a fan. And it is a good source of fiber.
Fascinating article, thank you. For breakfast I eat two eggs cooked in coconut oil with half an avocado. I also eat one tablespoon of organic coconut oil and 1400u D3 partway through the meal, as I read somewhere that D3 is better absorbed if consumed with fats, and coconut oil better consumer during a meal rather than alone, before or after. I’m happy with my 1 tbsp a day of coconut oil, it feels like the right amount for me, but after reading your article I’m wondering if I’m eating it with the best foods I could be, the eggs and avocado? Thank you.
I'd include some dark leafy greens too for sure!
It seems to me this question is easily answered. There are regions where people get 63% of their dietary energy from coconut.
“The habitual diets of the toll dwellers from both Pukapuka and Tokelau are high in saturated fat but low in dietary cholesterol and sucrose. Coconut is the chief source of energy for both groups. Tokelauans obtain a much higher percentage of energy from coconut than the Pukapukans, 63% compared with 34%, so their intake of saturated fat is higher. ”
http://ajcn.nutrition.org/content/34/8/1552.full….
Did the inhabitants of Tokelau suffer from MS historically? There is no record of this online.
Dietary fats are not FFAs, and medium chain FFas are cleared swiftly by the liver. The Sn- position of lauric acid on the triglyceride will also influence how much gut cells are exposed to the FFA.
I've be curious to see butyrate, SFCA and fiber intake of Pukapuka and Tokelau tribes…
I’m not sure if anyone has funded a study on said tribes to accurately deduce their MS rates. This would be extremely expensive, and historically, there was no knowledge of any modern diseases, and we thought the earth was flat, too.
What about using coconut oil as a moisturizer? Could it have a the same effects as does ingested as the research report suggests?
No. Coconut oil not be inflammatory if applied topically
Well I get a rash from it if I apply it on my skin. Seems not everyone does though. I’ve never noticed any problems from ingesting it, even now while my gut is inflamed due to dysbiosis and I react sensitively to many common foods. I would never think of putting it in tea though, and don’t drink coffee – I only use it to fry things and as a sauce for the many vegetables I eat now.
Good article Ben. Love the podcasts!
Have you seen the work of Dariush Mozaffarian on the effect of specific fatty acid fractions on insulin sensitivity and heart disease risk? It’s interesting stuff! See Good Fats, Bad Fats article at http://wp.me/p5VAQF-Y6
Also, I fully agree with the high fat, plant based, fibre rich approach. There’s a list of high fibre low insulin load foods in this article that may be of interest – http://wp.me/p5VAQF-XN .
Thanks Marty – I'll check them out!
Interesting. I have to admit that I have trouble getting enough vegetables. Don't of them raw upset my stomach (broccoli) and although I seem to cook a ton, they disappear so quickly.
I've been cooking bacon and eggs for breakfast, with about 30% vegetables mixed in. I then add about a tbsp of coconut oil for more fat and flavor. However, I also add between a tsp and tbsp of ground flax seed at the same time. This seems to be one way to balance out the coconut oil with scfa, right?
Yep, that would work! But get some leafy greens in there too. Not just broccoli or flax.
Great article but again the solution is simple, Balance is the key, coconut oil is not the only oil in the world. I have 5 different oils that rotate around my diet, because to me I already found that coconut oil doesn’t agree with me in higher doses. Actually probably a high intake of any oil wouldn’t be good. I use pumpkin seed oil, olive oil, avocado oil, sunflower oil , grapeseed oil. One point to remember is that everything you apply or use made of coconut also counts, like moisturiser , shampoo etc…
Coconut oil and coconut butter (not the water or whole meat) causes intense rapid weight gain for me. I can put on 6 pounds after very small amounts, obviously water weight. Tried numerous times to incorporate the oil before I gave up. I stick to raw avocado, plus grapeseed and olive oil, for my primary fats. Noticed a few people posting on Marks Daily Apple with the same problem. (I am not primal or paleo; like you Ben, I continuously study nutrition and my own body)
FYI I read somewhere that diabetics also need to be careful with MCTs like coconut oil as insulin can be affected. I did not save the link but can probably be googled.
Interesting article. I went Paleo in 2010, implementing intermittent fasting, high fat, low carb regimens into my daily repertoire. I went from a mostly plant based diet, (low fat), to this high fat, low carb, moderate protein diet. Not only did I never lose weight, I actually gained some pounds, began experiencing a lot of gut dysfunction in 2013 (which is still present even after many trial and errors and mucho big bucks), thyroid nodules were discovered, went into premature menopause, as well as being in the exhaustive phase of HPA axis dysregulation. I worked with a functional medicine doc who placed me on a ketogenic diet. Again, no weight loss, lethargic, just overall feeling puny. I did an elimination diet which was mostly plant based, moderate fat (30%), moderate protein. I lost weight, I had so much energy, I felt great. The take away, as you said, is balance. I believe we also are genetically so different from one another. Who is to say that one diet fits all? That is definitely not the case. As I’m writing this, I just finished (I’m a nurse who has recently gone back to night shift) my bullet proof coffee with 2 tbsp of coconut oil, and 2 tbsp of grass fed gelatin, I’m beginning to realize it’s time to shift my paradigm once again, and go back to what worked for me in the first place. I love Paleo because it helped me learn the art of Whole Food preparation, but Paleo is not the panacea for all people that it claims to be. I believe it’s been very damaging to my body overall as I’ve tried to fit myself in this box that is clearly not cut for me. I really appreciate this article.
Paleo is for type o blood
C’mon, the blood group diet is utter bullshit. The groups split millions of years ago, monkeys have them too, how could they have anything to do with our modern agricultural diets?
And yes, maybe paleo isn’t a one size fits all diet, but what we should take from it is the basic principle of looking at which kinds of foods evolution has adapted us to eat. Obviously this will vary a bit from person to person and we have to listen to our bodies a bit too.
I recently tried monolaurin but had to quit after a couple weeks due to fatigue and brain fog. They described this as”herxeimer” effect in the site. Now I’m wondering if there’s another explanation. Any ideas? I was trying a very low dose.
Yeah, herxheimer is a detox reaction HOWEVER, sometimes it can simply be because you restricted carbs a bunch once you started into extra coconut oil. Lots of moving parts here. I'd be happy to help you via a personal one-on-one consult. Just go to https://bengreenfieldfitness.com/coaching. and then choose a 20 or 60 minute consult, whichever you'd prefer. I can schedule ASAP after you get that.
Per #Dr Amy Yasko in her Chapter 6, she wrote that some people are sensitive to the MCT oils in coconut oil due to certain genes> I get that brain fog too & is not good. Then comes OCD, increased ADHD and people & family will ask what’s wrong with me during this time. I also get HEAT Flushes and raised body temp the entire time i eat Coconut Oil. I just COOLED off after 15 years by starting LDN. I found out LYME was one reason for feeling constantly over-heated. So i don’t want that feeling back. I prefer foods that help COOL my inflammation. http://www.dramyyasko.com/wp-content/files_flutte…
Also, Coconut is High in Arginine (bad for herpes & EBV viruses), high in Copper (bad for copper sensitive folks) and some brands I read might be high in mold toxins IF it’s not processed a certain traditional way like Tropical Traditions brand or sit on store shelves too long. Research more on that.
Yes, it’s also interesting that Terry Wahl’s protocol includes lots of coconut oil, esp for inflammation/MS etc. Her 3rd level (most intense for ridding oneself of MS) especially has quite a bit of coconut and coconut oil. She doesn’t really use MCT oil tho…
Hi Ben
Very concerning article here.
I notice in previous articles/podcasts/interviews etc you have advocated liberal use of coconut oil and other products; in one case recommending 8-10 tablespoons per day of coconut oil for someone trying to gain muscle on a lowcarb/ketogenic diet.
Do you still recommend that high of a daily dose of oil, and others such as coconut milk/cream in foods, or have you really backed off doses that high?
I'm trying to get closer to 2T per day based on this latest research, and also ensuring that I focus on continuing to take in adequate fiber/veggies!
I hope (if not already) you will read Dr Mary Newhart’s book(s) about the results of coconut oil in helping dementia. It seems the insulin resistant brain can use ketones for fuel.
IT’S ALL.ABOUT BALANCE !!!!
SOME PEOPLE JUST TAKE THE EXTREME PATH
MODERATION FOLKS
COCONUT OIL AND OTHER COCONUT OIL PRODUCTS LIKE MCT OIL XCT OIL BRAIN OCTAIN OIL COCONUT MILK COCONUT CREAM ETC MUST BE USED LIKE ANYTHING IN MODERATION …. SO LET’S NOT RING THE ALARM BELL PLEASE !!
Wow thanks for the article Ben. I've been consuming at least 4-6 TBS of coconut oil everyday to hit my fat goals. Thankfully I've already been including macadamia nuts, walnuts, grassfed cow butter, and fibrous veggies. Would you suggest scaling it down for a few weeks before consuming this much coconut oil again?
Best way to know is to test. Test inflammation, triglycerides and a gut test for SCFA's specifically. That way you know for sure. If it were me, I'd just do a quick 7-10 day "cleanse" primarily plant-based, water, etc. before jumping back into a level of coconut oil intake closer to 2T.
Great Article Ben. Ensuring we get as many vegetables as we can is really critical. Also, it's worth nothing that cauliflower, broccoli, kale, collards are all from the same family. So I bet most of us, me included, eat mostly veggies from these related plants. It's important to find ways to branch out and get many varieties of vegetables, which some of us don't always do. I'm enjoying your recent articles quite a bit.
So, eat the coconut oil with lots of veggies with fiber (+ the vitamins, minerals and anti-oxidants in there don’t hurt either) and make sure we consume lots of fiber from flax, chia, etc?
Otherwise we are good to consume 1-4 TBsp/day?
Yes, although it still may be prudent to avoid exceeding two tablespoons per day for extended periods of time and to "count" your MCT oil intake too as part of that.
Maybe someone could help shed some light on this for me: I don’t seem to respond well to consuming coconut oil. I don’t believe it is a food sensitivity/allergy. My body does not seem to be able to use coconut oil as energy very effectively. I feel less energized when I eat coconut oil. And it does not seem to be helpful to me re: weight loss or getting into ketosis. I’ve tried doing a lot of things that one is supposed to do to become a “fat burner” instead of a “sugar burner” and a lot of those seem to leave me feeling bad and tired; coconut oil and a “keto” diet seems to be kind of the worst offenders for me. I know that there is supposed to be some kind of a transition period that lasts for maybe a few weeks between being a sugar burner and becoming a fat burner; I tried for many months and could just never achieve fat burner status and the longer I tried the worse I felt. This is a bit of an overly dramatic comparison, I know, but it kind of seems like for me, consuming a tablespoon of coconut oil is a bit like someone else consuming a tablespoon of crisco shortening – my body just can’t seem to burn the stuff. I know the obvious answer for me re: coconut oil is just don’t consume it but I also I feel like the thing with coconut oil might be some kind of a clue to something bigger that might be going on with my metabolism – but I can’t figure it out. I also can’t seem to figure out a way of eating that works for me, long term. I really want to be a fatburner, but it almost feels like that “gear” is missing for me.
In short: you may have a coconut allergy. I'd look into a good food allergy testing service such as Cyrex labs.
The missing “gear” may be carnitine which is used to transport fats into ones cell mitochondria. I prefer Acetyl-L-Carnitine and I sometimes sense a noticeable increase in body temperature when I take it.
Hey, so does this same thing happen when consuming much longer chain of fatty acid like fats from animal such as lard, tallow, marrow (longer than LA C12)?
Also, as I was reading some previous article on doing low carb, you mentioned consuming organs such as liver & sweetbread in order to help with hormone such as thyroid, citing part of an interview on Chris's podcast where northern indigenous people eat moose thyroid glad. You do know that sweetbread is thymus or pancreas and not thyroid right? It seems that selling thyroid gland (gullet trimming) itself is illegal as there has been a case of toxicity even when consuming in small amount. What does this all means? Indigenous people were eating thymus and thymus somehow help with thyroid?
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC18329… https://www.paleohacks.com/thyroid/eating-thyroid…
It's definitely still recommended to eat plenty of vegetables if you're eating lots of animal meats/fats too, although the same research does not (to my knowledge) exist for animal fats of longer chain variety. Also (and I covered this in detail on a podcast), thyroid glandular is indeed included as a category of sweetbreads. But i personally use and recommend "Thyrogold" supplement for things like that.